BDNF (Brain Derived Neurotrophic Factor) − AN EXTRAORDINARY AND POWERFUL MASTER REGULATOR OF THE BRAIN
THE INCREDIBLE CASE OF HENRY MOLAISON − THE AMNESIAC WE WILL NOT FORGET
 In 1953, Henry G. Molaison, 27, from Manchester, Connecticut (USA) underwent a major bilateral anteromedial temporal lobectomy, with extensive resection of the anterior 2/3 of the hippocampi, parahippocampal cortices, entorhinal cortices, piriform cortices, and amygdalae (FIG. 1), in an attempt to stop his severe, worsening, drug-resistant, tonic-clonic seizures (15-20 per day), which had afflicted him since childhood and had probably been caused by a road accident at the age of 9, which had resulted in a fractured skull and brain concussion.
In 1953, Henry G. Molaison, 27, from Manchester, Connecticut (USA) underwent a major bilateral anteromedial temporal lobectomy, with extensive resection of the anterior 2/3 of the hippocampi, parahippocampal cortices, entorhinal cortices, piriform cortices, and amygdalae (FIG. 1), in an attempt to stop his severe, worsening, drug-resistant, tonic-clonic seizures (15-20 per day), which had afflicted him since childhood and had probably been caused by a road accident at the age of 9, which had resulted in a fractured skull and brain concussion.
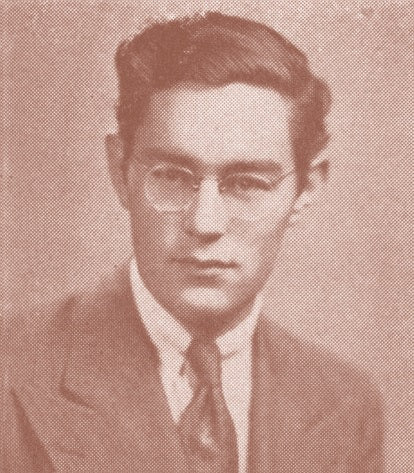
Henry G. Molaison (1926-2008).
Photograph taken 2 years before his bilateral anteromedial temporal lobectomy.
− One of the most widely studied patients in the History of Medicine.
– I quote Dr William B. Scoville, the expert neurosurgeon who had operated on him: “(…) we performed a bilateral resection of the medial temporal lobes, advancing posteriorly for a distance of 8 cm from the central point of the edge of the temporal lobe, so that the temporal horn formed the lateral margin of the resection”.
The neurosurgeon had already performed several partial ablations of other areas of the brain in cases of severe psychosis (at that time they were defined as “psychosurgery procedures”) with no significant side effects (Scoville, 1951). – The procedure carried out on Henry Molaison had had a favourable impact on his epileptic fits, which were considerably fewer and of shorter duration, but the patient had become incapable of creating new memories: he only had a blurred memory of a few events concerning his family and childhood; nevertheless, he could play the piano, ride a bicycle and perform even complex actions that the brain transmits to the somatic musculature due to conditioned motor patterns, “motor memories”, which are currently defined as “intuitive”, but which the patient did not remember having learned.

a) Extensive ablation of the anterior 2/3 of the hippocampi, parahippocampal cortices, entorhinal cortices, piriform cortices, and amygdalae;
b) Normal brain.
Top: Inferior view of normal encephalon.
Bottom: Cross section at the level of the temporal lobe of Henry
Molaison’s brain (a) and normal brain (b).
The patient's motor cortex, basal ganglia, and cerebellum were intact, therefore his coordinated automatic motor skills were correctly preserved. His ability to formulate procedural memory remained intact.
– Despite the severe memory problems, the patient performed well in intelligence and articulated language skill tests, a clear indication of how some memory functions – short-term storage (max. 1-2 minutes), vocabulary, phonemes, etc. – had not been compromised by the surgery (Corkin, 2002; Smith & Kosslyn, 2007).
Before the Molaison case, neuroscientists had considered memory to be "monolithic": the entire brain was involved in the memorisation processes. It is currently recognised that short-term memory is created by trains of electrical impulses conveyed from the cortex to the hippocampus, leaving no trace in the DNA of the hippocampal cells.
– If the experience is emotionally meaningful or repeated (repetita iuvant), the information stabilises, it is imprinted in the DNA of the hippocampal cells, which send engrams to the cortex that are now recorded and persist over time. This is how long-term memory is formed.
In the incredible case of Henry Molaison, the hippocampus and neighbouring cortices (FIGS. 1, 2) had been partially removed, which meant that “his” time had stopped on 1 September 1953, the date of his surgery; after that date ... nothing.
– From 1955, the patient was constantly monitored for a few hours a day by neuropsychologist Brenda Milner; every day – without exception – Henry could not remember ever meeting her before. Every day throughout the many years of observation, Henry would hold out his hand to her and introduce himself: “Hi… I am Henry, nice to meet you, Ma’am”.
Henry lived to the age of 82, in a temporary present moment, in the here and now... always and only for a few seconds, in a state of “perfect” mindfulness.
• The recent past did not exist, the future would never be remembered; there was only the fragmented remote past, which was in any event prior to the date of his surgery.
– In 2014, Molaison’s brain became the focus of very detailed, sophisticated studies (Annese et Al., 2014); it is now preserved at the San Diego School of Medicine Institute for Brain and Society Brain Observatory, San Diego, California (USA) (2401 very thin fronto-occipital “slices”; inter: 70 mm).
From these studies it emerged that the amount of brain tissue removed was less than what was reported at the time, but... there was no post-surgery NMRI in 1953.
– Even after his death, neuroscientists continue and will continue to learn from the “amnesiac we will not forget”, which is the title of an article by Benedict Carey published in the New York Times on 4 December, 2008.
Paradoxically, the man without a memory is and will continue to be a lasting memory for all neuroscientists, and others.
BIZZOZERO’S ERROR AND THE NEUROTROPHINS
According to the classification formulated in 1894 by Giulio Bizzozero (1846-1901) (Vigliani, 2002), the cells of an organism can be divided into 3 groups:
- labile, which continuously reduplicate, for example the mucous membranes, epidermis and endometrium (lining epithelial cells);
- stable, which do not normally reduplicate continuously, but can undergo mitosis in response to homoeostatic requirements, for example in glandular tissues or in the liver after a hepatectomy;
- perennial, highly specialised, incapable of cell division, for example nerve cells.
This classification, which was used until the final decades of the last century (Chiarugi & Bucciante, 1968), was later radically deconstructed following the discovery of Nerve Growth Factor (NGF) (Levi-Montalcini & Hamburger, 1951).
NGF is a peptide-based neurotrophic factor primarily involved in the proliferation, growth, maintenance and survival of some target neurons.
- Bizzozero’s perennial cells… do not exist.
The following belong to a group of Neurotrophic Factors not related to NGF: 1) CNTF (Ciliary NeuroTrophic Factor); 2) GDNF (Glial-cell-line Derived Neurotrophic Factor); 3) TGFα/b (Trophic Growth Factor α/b); 4) FGFs (Fibroblast Growth Factors); 5) EGF (Epidermal Growth Factor) and 6) PDGF (Platelet-Derived Growth Factor).
Since NGF, 3 further neurotrophins (NTs) have been discovered in humans: BDNF (Barde et Al., 1982), NT3 (Maisonpierre et Al.,1990) and NT4 (NT4/5) (Hallbook et Al., 1991), each with a distinct profile of trophic effects on specific central and peripheral neuronal subpopulations.
Of particular significance is BDNF (Brain Derived Neurotrophic Factor), which was first isolated by Yves-Alain Barde, Dave Edgard & Hans Thoenen in the laboratories of the Neurochemistry Section of the Max-Planck Institut für Psychiatrie in Munich - Germany.
The research group was coordinated by the Swiss Prof. Thoenen. – There follows a quote from part of his original description of the discovery of BDNF: “(…) we are reporting on the purification of a factor, taken from the brain of pigs, which promotes the survival and growth of the sensory neurons in cultured chicken embryos (…); approximately 1 microgramme of this factor was isolated from 1.5 kg of pig brain (5 brains, Ed.); this factor is the first purified neurotrophic factor since NGF (Nerve Growth Factor), from which it can be clearly distinguishable due to its different antigenic and functional properties”.
Thoenen studied Neurotrophic Factors throughout his life (Thoenen, 1995, 2000; Thoenen & Sendtener, 2002), “a modest man whose discoveries have had profound impact on modern neuroscience” (Iversen, 2013).
A human brain should contain, on average 0.85 ≈ microgrammes (one microgramme = a millionth of a gramme).
Mature BDNF is a protein composed of 119 amino acids, with a molar mass of 14 KDa ≈ (13.2-15.19 KDa), an isoelectric point of 9-10 (Chao & Bothwell, 2002). It shares 50% of its amino acid sequence with 3 other NT (Narhi et Al., 1993; Marco Salazar, 2014) (FIG. 3).

The hippocampus is very difficult to successfully identify in anatomical dissection. This is because it is located deep in the temporal lobe, and because there are some differences in the terminology used by the various schools of anatomy. Moreover, its course does not follow the major axis of the temporal lobe, but is inclined from bottom to top and from the outside to the inside. − Its correct location is shown on the 3 images. left hemi-encephalon: a) temporal gyrus; b) hippocampal gyrus; left semi-encephalon: a) temporal lobe, anterior portion; b) empty space that accommodates head and body of hippocampus; c) hippocampus sectioned 2/3 anterior - 1/3 posterior (tail); d) fimbria of hippocampus; a) head and body of hippocampus; b) fimbria of hippocampus. − Note that the hippocampi of the 2 hemispheres approach the midline and, in the region of their tails, they are paired; (c) tentorium of hippocampus.
Once attached to its main TrKB receptor, a dimer, BDNF initiates 3 distinct PATHWAYS. From top, left: in the 1st PATHWAY, the sequential concatenation of 5 protein complexes (Shc, Grb2, Sos, GAB1, PI3K) stimulates PIP2, a phospholipid component of the cell membranes, which − in turn − stimulates another phospholipid, PIP3. Through the intermediation of PDK1 (Phosphoinositide-dependent kinase) this produces AkT, also known as Protein-Kinase B. This facilitates neuronal survival, neuronal growth, neuroplasticity, and short-term memory (cytoplasmic activity). AkT can enter the nucleus and modify the DNA: in this case the information materialises in the long-term memory. −In the 2nd PATHWAY, intramembrane PIP2, stimulated by PLCγ, a protein attached to the 2nd arm of the TrKB dimer, stimulates IP3, which releases Ca++ and produces CAMK (or MAMK), a Ca++/modulin-dependent protein-kinase that enters the nucleus (see above for AkT). − The 3rd PATHWAY involves the sequential linking of the first 4 protein complexes to a series of promoters, as far as ERK (signal-regulated extra cellular kinase; it also enters the nucleus to modify the DNA). • NOTE: the table shows 2 TrKB receptors for display and graphic purposes only. In reality, the 3 PATHWAYS occur simultaneously following the interaction of BDNF with the TrKBs found on the neurons that expose them.
All 4 human NTs share a common ancestral gene (Dos Santos et Al., 2011; Covaceuszach et Al., 2021).
BDNF is encoded by the BDNF gene which, in humans, is located on chromosome 11, band p 13.
The BDNF gene is made up of 11 exons (exon = portion of the gene that is transcribed by RNA polymerases during transcription) associated with 8 functional promoters + 1 exon that codes for BDNF (Metsis et Al., 1993; Timmusk et Al., 1993).
The significance of this complex transcriptional organisation is not well understood; the most accredited hypothesis is that it induces multiple stages of regulation by means of alternative promoters, different RNA stability or different subcellular localisations of both RNA and proteins.
BDNF is synthesised in the neuronal endoplasmic reticulum as a PRE-PRO-BDNF complex which subsequently migrates into the Golgi apparatus and later into the trans Golgi system, a maturation system that faces towards the internal portion of the cell membrane.
The PRE portion (18 amino acids) undergoes proteolytic cutting in the endoplasmic reticulum of the nerve cell. Mature BDNF subsequently splits from the PRO portion (112 amino acids) due to the action of enzymes found in both the
intracellular and extracellular compartments.
If this latter splitting does not occur, mature BDNF is not formed. Instead the PRO-BDNF precursor is formed, and biological activity of this differs from that of mature NT (Lee et Al., 2001), which induces a neurotoxic effect, as occurs in Alzheimer- Perusini disease (Chen et Al., 2017; Fleitas et Al., 2018).
Each NT binds to one or more tropomyosin-kinase receptors, member(s) of the tyrosine-kinase family (TrKs) (Patapoutian & Reichhardt, 2001), which activate a wide range of intracellular signals, including – crucially – cyclic AMP phosphorylation (Ji et Al., 2005). • In the case of BDNF, it binds and activates 2 different transmembrane receptors, both at the pre-synaptic and postsynaptic level: one with high affinity [TrK (pronunciation: Trak) B], mentioned above, the other belonging to the TNF superfamily (Tumour Necrosis Factor), p 75, with low affinity.
• These 2 receptors show no homology, or cytoplasmic domain, and they activate different signalling pathways. They probably appeared at different times in the course of evolution (Tettamanti et Al., 2010).
In the presynaptic neuron, BDNF is “packed” into dense, optically dark vesicles; it reaches the terminal plate of the neuron (nerve plate) through rapid axonal flow from the neuronal nucleus (Conner et Al., 1997).


– Upon arrival of the electrical impulse (spike), BDNF binds to the 2 post-synaptic element receptors mentioned above, and there it triggers – on TrKB – 3 pathways, with distinct cascade mechanisms. TrKB is a transmembrane receptor with a short outer part and a long inner part, and is also a dimer (Shen & Maruyama, 2012) (TAB. 1).
– 1st PATHWAY: in an 8-step process [2 of which occur inside the neuronal plasma membrane (PIP2→PIP3)] we arrive at the formation of Akt, also known as Protein-Kinase B: this induces survival, neuronal growth and neuroplasticity whether it remains in the cytoplasm or enters the nucleus, and stimulates transcription → translation with the help of DNA.
– 2nd PATHWAY: CAMK (Ca2+/modulin-dependent kinase) is synthesised in a 4-step process. This enters the nucleus directly and – from this moment on – works in the same way as Akt in the 1st Pathway, in the intra- nuclear passage.
– 3rd PATHWAY: a 7-step process [the first 4 of which are identical to those of the 1st Pathway (Shc, Grb2, Sos and GAB1)] results in the synthesis of ERK (Extracellular Signal- Regulated Kinase). The terminal linking of 3 proteins (Ras, Raf 1 and MEK) to form a chain, identical to that which causes insulin to release glucose to the cells, thanks to DNA, also leads to the same effects as the 1st Pathway, thus highlighting the classic phenomenon of redundancy, as occurs in the cytokines (Milani, 2007).
• Synthesis: BDNF = neuronal survival, neuronal growth, neuroplasticity, neo-neurogenesis and prevention of neuronal apoptosis.
SPECIFIC NATURE OF BDNF
- Its activity on the post-synaptic receptor depends only on the depolarisation of the pre-synaptic neuron (Mowla et Al., 1999; Goggi et Al., 2003).
- It can be transferred per se from a donor neuron to a recipient neuron (role of neurotransmitter too?) (Kohara et Al., 2001; Selvam, 2018).
- It excites the glutaminergic synapses and depresses the GABAergic synapses (hence the excitation) (Tanaka et Al., 1997).
– In Henry Molaison’s hippocampi and neighbouring cortices, BDNF was overexpressed following his road accident, which explains his continuous, severe epileptic seizures and justifies the subsequent anteromedial temporal lobectomy with excision of part of both hippocampi.
The activities performed by BDNF are the most widely, best characterised of the 4 known NTs.
From the extensive medical-scientific literature consulted, the biological activities related to BDNF are: neuronal survival, neuronal differentiation, synaptogenesis, synaptic plasticity, increase in the arborisation of dendrites and new axons: a truly... extraordinary, powerful master regulator of the brain, both in prenatal life and throughout life (TAB. 2).
In the brain, a high concentration of BDNF can be detected in the cerebral cortex, especially the pre-frontalcortex, which is well-developed only in humans (Milani, 2018), in the cerebellum, the basal ganglia and – above all – the hippocampus, structure belonging to the limbic brain; outside the brain, in the retina, kidneys, heart, lungs, pancreas, prostate, skeletal muscle, and saliva (Pruunsild et Al., 2007).

Not bad for a protein made up of only 119 amino acids.In the prefrontal cortex... for high level thinking, in the cerebellum... for posture, in the basal ganglia... for the control of extrapyramidal involuntary movements and in the hippocampus... for the consolidation of long-term memory and the control of emotions.
− Binomial Prefrontal Cortex-Hippocampus… for learning.
BDNF has been synthesised in all vertebrates since the lower Carboniferous period, 360-318 million years ago, and is almost identical in all mammals. It has shown extraordinary success in the course of evolution (molecular stability and highly performing activities concerned with integration in the environment) (Götz et Al., 1992; Tettamanti et Al., 2010).
However, there are two factors that compromise BDNF function; a single substitution of methionine instead of valine (BDNF val66met) along its amino acid sequence has been linked with the susceptibility, incidence and clinical picture of certain psychiatric disorders (anxiety, depression) and neurodegenerative disorders such as glaucoma, multiple sclerosis, Alzheimer-Perusini disease, amyotrophic lateral sclerosis, Parkinson’s Disease and Rett Syndrome* (Egan et Al., 2003; Shen et Al., 2018).
BDNF val66met (variant) polymorphism occurs in 30% ≈ of the population (source: University of Milan - La Statale Insalutenews 19 October 2016) and is not associated with serum BDNF (Terraciano et Al., 2013).
The other genetic error is BDNF L21, associated with congenital central alveolar hypoventilation syndrome (Weese- Mayer et Al., 2002) (“Ondine’s curse”), a rare disease characterised by a major defect in the central control of respiration.
These genetic errors have only been demonstrated in humans.
Some changes in BDNF levels lead to psychiatric disorders, depression, bipolar disorders, psychosis, eating disorders, post-traumatic stress disorder, anxiety disorders, self-harm, and suicidal behaviour.
Of all the NTs, it has emerged that BDNF is the major regulator of many neuronal types such as sensory neurons, retinal ganglion cells, spinal motor neurons, cholinergic neurons, and some clusters of dopaminergic neurons.
BDNF is widely distributed in the CNS; its expression is decreased in many degenerative diseases, as demonstrated in post-mortem studies on Alzheimer-Perusini disease (Phillips et Al., 1991; Hock et Al., 2000), Parkinson’s disease (Mogi et Al., 1999; Phillips et Al., 1999), Huntington’s disease (Ferrer et Al., 2000), and severe depression (Lee & Kim, 2010), in which BDNF increases as a result of antidepressant therapy (Shimizu et Al., 2003).
Many neurons are eliminated during the period of intrauterine development in mammals: a large percentage of neurons already formed (20% to 70%) undergoes degeneration; this takes place in order to regulate the optimal number of neurons in adult life. However, this number changes significantly throughout life: at the age of 50 years ≈ most of the neurons in the hippocampus are replaced ex novo and new neurons are formed, along with the associated dendritic arborisations and synapses. This is to prevent the loss of memories that the apoptotic neurons had preserved as engrams: the master regulator of these complex functions is – above all – BDNF. – In fact, in the animal model of learning and memory, electrical stimulation of the hippocampus increases the expression of BDNF and NGF (Patterson et Al., 1992; Castrén et Al., 1993; Bramham et Al., 1996).
Optimal cognitive function is dependent on dynamic, active neuronal plasticity (Herndon et Al., 1997; Morrison & Hof, 1997; Gonzalez et Al., 2016), but over the years this cracks, mainly due to the loss of dendritic spines (Morrison & Hof, 1997).
This does not take place in the entire brain, but only in some specific areas: in cerebral ageing, neuronal loss is a phenomenon localised in the cortical, subcortical (Smith et Al., 2004) and hippocampal neurons, where a high concentration of BDNF is expressed (Erickson et Al., 2010).
This is the rationale for the progressive decline in voluntary and involuntary motor function, learning, memory and processing- critical thinking in many elderly people (Silhol et Al., 2008), in which a transition from neuro-inflammation to neuro- degeneration has begun (Milani, 2014, 2016; Milani & Pelosi, 2016; Montenero & Milani 2019) and/or atherosclerosis/ arteriosclerosis of the cerebral vessels (Vascular dementia).

The primum movens is Low-Grade Chronic Systemic Inflammation. This is the “silent killer” to be identified and neutralised, nothing else.
BDNF − NON-PHARMACOLOGICAL THERAPY
The conventional therapies currently available to reduce the phenomenological aspects of cerebral ageing are both pharmacological and non-pharmacological; the former, which target the neurotransmitters, with no guarantee of success, have various side effects and are expensive (Uberti & Molinari, 2018).
The gene expression of BDNF can be affected by a series of stimuli:
- Endurance motor exercise increases BDNF levels by 200%- 300% (Salfert et Al., 2010).
- Strength motor exercises [e.g.. repeated weight lifting for 5-10 min/day (Neeper et Al., 1995)]. The increase in BDNF in skeletal muscle is proportional to contractile intensity in aerobiosis relating to a more favourable fat/lean mass ratio, which is enhanced by the consumption of fatty acids for oxidation, and by the improvement in energy consumption of glucose (Mattheus et Al., 2009; Henry et Al., 2018).
- Deep sleep (Eckert et Al., 2017).
- Light stimulation: BDNF increase in the visual cortex (Castrén et Al., 1992).
- Osmotic stimulation: BDNF increase in the hypothalamus (Castrén et Al., 1995; Dias et Al., 2003).
- Meditation, Yoga (Cahn et Al., 2017), Mindfulness (Gomutbutra et Al., 2020).
- Ketogenic diet (Vizuete et Al., 2013).
- Intermittent fasting (Mattson et Al., 2020).
- Foodstuffs: Polyphenols (coffee, green tea, dark chocolate, blueberries) (Gravesteijn & Mensink, 2021).
- Polyunsaturated fatty acids: Omega 3, Omega 6 (Wu, 2004).
- Probiotics containing Bifidobacteria (Intestine-Brain Axis) (Tian et Al., 2019).
Avoiding patho-stress, social isolation, refined sugars and ethanol: these are powerful depressants that affect the production of BDNF.
BDNF − LOW-DOSE PHARMACOLOGICAL THERAPY
A therapeutic approach using BDNF could be extremely effective in preventing and treating neurodegenerative diseases (and others) (see above), which suffer from a deficiency of this crucial NT.
Knusel et Al. (Aut. cit., 1992) demonstrated that the administration of recombinant human BDNF in the cerebral ventricles of rats results in the neuroprotection of damaged cholinergic neurons.
Similarly, in 2001 (Chen et Al., 2001) it was demonstrated that intravitreal injections of BDNF in cats increased the survival of retinal ganglion cells after partial destruction of the optic nerve.
At the time it was believed that BDNF could not cross the Blood-Brain Barrier (BBB), a functional structure located between blood and brain parenchyma that selectively regulates blood flow to and from the brain, thus protecting it from intoxication and poisoning.
For this reason, experiments were necessarily designed as in loco procedures (e.g., as stated above, in the cerebral ventricles and the vitreous body), directly into the CNS.
– The discoverer of BDNF himself expressed scepticism about the rational therapeutic use of NTs (Thoenen & Sendtner, 2002).
This continued until 2010, when Klein et Al. (2010) brilliantly demonstrated that the blood concentration of BDNF reflected what was found inside the brain: BDNF did cross the BBB.
It did, however, present problems relating to the dose administered.
In this respect, the BDNF low dose formulation (4CH) successfully solves the problem. Uberti & Molinari (Aut. cit., 2018; Molinari et Al., 2020) demonstrate that BDNF 4CH (Guna Laboratories - Milan):
in vitro
- crosses the intestinal barrier;
- crosses the BEE, thereby reaching the brain tissue;
- activates the astrocytes and neurons, the 2 main types of cells involved in the ageing process;
- activates its main TrKB receptor through the recruitment of MAPK [(mitogen-activated-protein-kinase) (also defined as MAP = ERK)], a kinase that directs cellular responses to various stimuli, such as e.g. mitogens, osmotic stress, pro-inflammatory cytokines, etc. (Pearson et Al., 2001).
in vivo
- after the oral intake of BDNF 4CH, the drug arrives in the brain within 1 day, reaching a peak within 2 days;
- BDNF 4CH remains in the brain even in the absence of treatment, since it triggers the endogenous physiological systems that support the anti-ageing processes.
The authors conclude that “the use of low-dose BDNF offers a number of benefits due to the fact that this preparation has no side effects or adverse reactions, features that are necessary if it is used without the supervision of a specialist”.
In the section “BDNF – Non-pharmacological therapy”, I have also identified – among others – deep sleep, Omega 3/6 fatty acids and Bifidobacteria as being stimulants of BDNF gene expression.
– Therefore, for all patients who could benefit from taking Guna-BDNF (Brain Derived Neurotrophic Factor - human recombinant), 15-20 drops x 2/day by sublingual route for 4-6 months (children < 6 years of age: 10 drops x 2/day by sublingual route for 4-6 months) and, in general (TAB. 3):
- patients with neurodegenerative diseases (vascular and non-vascular dementia, Alzheimer-Perusini disease, Parkinson’s disease, multiple sclerosis, Huntington’s disease, Rett syndrome and others);
- Patients suffering from psychiatric diseases [anxiety (Malzac, 2002), severe depression, depression, autistic spectrum disorders, obsessive compulsive disorder, anorexia nervosa, bulimia nervosa, and others (Supino, 2020; Melcarne, 2021)];
- Specific learning disorders (Supino, 2019);
- Patients suffering from sarcopenia [BDNF is actively involved in muscle regeneration and in boosting the oxidation of fatty acids; BDNF is also produced directly in striated muscle, with a peripheral endocrine function (So et Al., 2014; Delezie et Al., 2019)];
- Cardiovascular diseases. BDNF stimulates angiogenesis and controls the survival of adult endothelial cells, vascular smooth muscle cells, and cardiomyocytes;
- Type 2 diabetes (Krabbe et Al., 2007; Meek et Al., 2013; Davarpanah et Al., 2021) ... ... my best advice is therapeutic supplement, with or without overlapping with conventional drugs, with:
Guna-Melatonin, 15-20 drops x 2/day;
Omegaformula – Omega 3-6-9 from micronised seeds of the Baobab fruit, 3 chewable tablets/day during or after main meals;
Proflora (probiotic component: Bifidobacterium and Lactobacillus genera), 1 sachet/day before lunch.
Guna-BDNF is also an effective treatment for mental fatigue, chronic fatigue syndrome and neurovegetative disorders due to long-COVID (post COVID-19 brain fog, or neuro- COVID).
All over the world, humans are living longer and seemingly healthier than just a few decades ago.
All this – however – must of course be set in the context of the basic biology of each individual, “his/her” medical history, “his/her” physiological and pathological ageing processes, “his/her” genetic programming [mitotic clock (Ehrenstein, 1998; Fossel, 2018)], “his/her” lifestyle, and the numerous, not always identifiable factors that play a part in making old age difficult – for many – and increasingly dependent on third parties.
Adding years to life is not the same as adding life to years.
Neurodegenerative diseases, especially Alzheimer-Perusini disease and other forms of dementia that result in the progressive loss of memory, elaborate thinking and purposeful behaviour have a negative impact on learned functioning and daily activities (emotional problems, semantic and lexical difficulties, memory loss, reduced motivation).
– This entire procession depends on the progressive atrophy of the cortical and subcortical regions that underlie the factual nature of these behaviours (including neuro-ageing).
These brain areas, which formed in humans as an accident of evolution, these 4 brains (Milani, 2018) are “orchestrated” by BDNF which “does not marry the soma as such; it rests on that and it is from that position that it can put together the less perfect products of corporeality, turning them into Regulation” (Turco & Turco, 2019).
– It is “ageing”, impoverished BDNF that withers the hippocampus and the cortices that “communicate” with it (and ... vice versa); it is lipofucsin, neuromelanin, the Lewy and Hirano bodies, the substance b-amyloid and the Tau proteins that interrupt the neurotransmission wires.
– BDNF 4CH opens up new scenarios, new and real hopes, revitalises ageing life, breathes life into destiny, takes the edge off... “Hi, I am Henry, nice to meet you, Ma’am”.
I dedicate this work in memoriam to my dear friend Dr Marlowe Elizabeth Reynolds of Berwyn, Chicago, who recently passed away.
− Marly... this goes for you.

